Symptoms and Diagnosis of Stage 3 CKD
Chronic Kidney Disease (CKD) progresses through various stages, each with distinct symptoms and diagnostic criteria. Stage 3 CKD, marked by a moderate decline in kidney function, stands out due to its noticeable symptoms and specific diagnostic methods. Understanding Stage 3 CKD is essential for effective management and treatment.
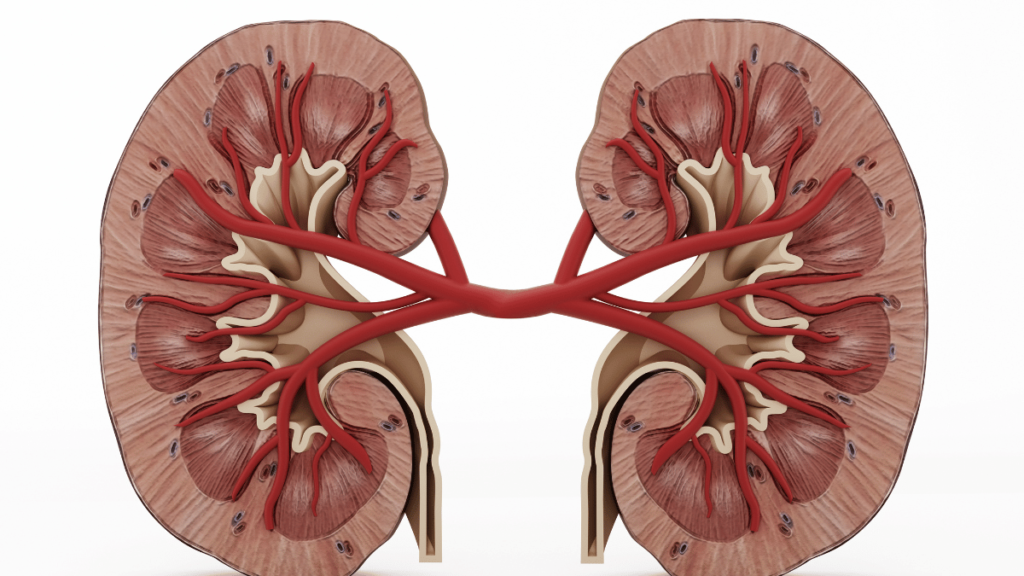
Understanding Stage 3 CKD
Stage 3 CKD is characterized by an estimated Glomerular Filtration Rate (eGFR) between 30 and 59 mL/min/1.73 m². This stage is divided into two sub-stages: 3A, with an eGFR of 45-59, and 3B, with an eGFR of 30-44. The moderate reduction in kidney function at this stage often leads to more apparent symptoms compared to earlier stages.
Symptoms of Stage 3 CKD
As kidney function decreases, individuals with Stage 3 CKD may experience various symptoms that impact their daily life. Common signs include noticeable fatigue and weakness, often resulting from anemia related to kidney dysfunction. Swelling, or edema, in the legs, ankles, or feet is another frequent symptom, caused by fluid retention.
Changes in urination patterns, such as increased frequency or changes in urine color and consistency, can also occur. Some individuals may experience shortness of breath due to fluid buildup in the lungs, a condition known as pulmonary edema. Additionally, lower back pain or discomfort in the sides may be reported by those with Stage 3 CKD.
Distinguishing Stage 3 CKD from Other Stages
When comparing Stage 3 CKD to other stages, several key differences emerge. In Stage 1 CKD, with an eGFR of 90 or higher, individuals typically do not experience symptoms, and the condition is usually identified through abnormalities in blood or urine tests. Stage 2 CKD, characterized by an eGFR between 60 and 89, also presents minimal symptoms but requires regular monitoring to manage kidney damage.
In contrast, Stage 4 CKD, with an eGFR between 15 and 29, involves more severe symptoms, including significant fluid retention and anemia, and necessitates planning for dialysis or a kidney transplant. Stage 5 CKD, marked by an eGFR below 15, presents severe symptoms such as extreme fatigue and nausea, often requiring dialysis or a kidney transplant to sustain life.
Diagnosing Stage 3 CKD
The diagnosis of Stage 3 CKD involves several key tests and evaluations. Blood tests are used to measure eGFR and serum creatinine levels, providing insight into kidney function. Urinalysis helps detect protein or blood in the urine, which can indicate kidney damage.
Imaging studies, such as ultrasounds or CT scans, may be employed to visualize kidney structure and identify any abnormalities. In some cases, a kidney biopsy may be necessary to determine the underlying cause of kidney damage.
Common Symptoms of Stage 3 CKD
Stage 3 Chronic Kidney Disease (CKD) presents with a range of symptoms that are more noticeable compared to earlier stages. Individuals often experience significant fatigue and weakness due to anemia, which is a common consequence of reduced kidney function. Fluid retention can lead to swelling, particularly in the legs, ankles, and feet.
Changes in urination patterns are also typical, with individuals reporting increased frequency or alterations in urine color and consistency. Additionally, some may experience shortness of breath, a result of fluid accumulation in the lungs. Discomfort or pain in the lower back or sides can also occur, reflecting the strain on the kidneys.
Diagnostic Tests and Procedures
Diagnosing Stage 3 CKD involves a series of tests designed to evaluate kidney function and structure. Blood tests play a crucial role, measuring eGFR and serum creatinine levels to determine the extent of kidney impairment. Urinalysis is employed to detect abnormalities such as protein or blood in the urine, which indicate kidney damage. Imaging studies, including ultrasounds or CT scans, help visualize the kidneys and identify any structural issues. In certain cases, a kidney biopsy may be performed to gain insight into the underlying causes of kidney damage.
Importance of Early Detection
Early detection of Stage 3 CKD is vital for effective management and to slow disease progression. Identifying CKD in its early stages allows for timely intervention, which can significantly improve outcomes and prevent complications. Regular monitoring and proactive management strategies can help preserve kidney function and enhance quality of life.
Addressing CKD early also provides an opportunity to make necessary lifestyle changes and start appropriate treatments, which can alter the disease’s trajectory.
Common Causes of Stage 3 Chronic Kidney Disease
Stage 3 CKD can arise from various underlying conditions that cause gradual kidney damage. Common causes include diabetes, which leads to diabetic nephropathy, and high blood pressure, which can damage blood vessels in the kidneys. Other significant contributors include chronic glomerulonephritis, an inflammation of the kidney’s filtering units, and polycystic kidney disease, a genetic disorder causing fluid-filled cysts in the kidneys. Each of these conditions can impair kidney function over time, leading to Stage 3 CKD.
Risk Factors and How They Contribute
Several risk factors can increase the likelihood of developing Stage 3 CKD. These include a family history of kidney disease, which can predispose individuals to inherited conditions affecting kidney function. Age is another significant risk factor, as kidney function naturally declines with advancing age. Lifestyle factors such as obesity, smoking, and a sedentary lifestyle also contribute to CKD risk. Additionally, pre-existing conditions like cardiovascular disease and high cholesterol can exacerbate kidney damage, accelerating the progression to Stage 3 CKD.
Treatment and Management Strategies
Lifestyle Changes and Diet Recommendations
Managing Stage 3 CKD effectively involves making significant lifestyle changes and adopting a kidney-friendly diet. Patients are encouraged to follow a balanced diet low in sodium, potassium, and phosphorus to reduce kidney strain. Regular physical activity is recommended to help manage weight and improve overall health.
Avoiding smoking and limiting alcohol intake are also crucial steps in reducing kidney-related complications. Personalized dietary plans, often developed with the help of a dietitian, can help manage symptoms and support kidney function.
Medications and Medical Interventions
In addition to lifestyle changes, medications play a critical role in managing Stage 3 CKD. Medications may be prescribed to control blood pressure, manage blood sugar levels in diabetic patients, and reduce cholesterol. Phosphate binders and erythropoiesis-stimulating agents may also be used to manage related complications such as anemia and abnormal phosphate levels.
Regular consultations with healthcare providers are essential to adjust medications as needed and address any emerging issues.
Monitoring and Managing Progress
Ongoing monitoring is essential for managing Stage 3 CKD and preventing further progression. Regular follow-up appointments allow healthcare providers to track kidney function, assess the effectiveness of treatments, and make necessary adjustments. Routine blood tests, urine tests, and imaging studies are part of this monitoring process.
Effective management requires a collaborative approach between patients and healthcare providers to ensure that treatment plans are adapted to changing conditions and to address any new symptoms promptly.
What to Expect in Stage 3 CKD

The prognosis for individuals with Stage 3 CKD depends on various factors, including the underlying cause of the disease, the effectiveness of treatment, and adherence to lifestyle changes. With appropriate management, many individuals can maintain a good quality of life and slow the progression of CKD.
Regular monitoring and proactive care are crucial in achieving better long-term outcomes. While Stage 3 CKD indicates moderate kidney impairment, early intervention can significantly impact the future course of the disease.
Potential Complications and How to Address Them
Stage 3 CKD can lead to several potential complications if not properly managed. These may include worsening kidney function, cardiovascular problems, and electrolyte imbalances. To address these complications, it is essential to adhere to prescribed treatments, make necessary lifestyle adjustments, and attend regular follow-up appointments.
Healthcare providers may offer additional interventions or adjustments to treatment plans to manage complications effectively and prevent further deterioration of kidney function.
Conclusion
Stage 3 Chronic Kidney Disease (CKD) represents a critical point in the progression of kidney disease, characterized by moderate impairment of kidney function. Recognizing and understanding the symptoms of Stage 3 CKD, such as fatigue, swelling, and changes in urination, is crucial for early intervention and effective management.
Diagnostic tests, including blood tests, urinalysis, and imaging studies, play a key role in accurately assessing kidney function and determining the appropriate course of treatment.
Addressing the common causes and risk factors associated with Stage 3 CKD, such as diabetes, high blood pressure, and lifestyle factors, is essential for preventing further progression. Implementing lifestyle changes, adhering to dietary recommendations, and using medications as prescribed are integral to managing the condition and improving outcomes.
Ongoing monitoring and proactive management are necessary to mitigate potential complications and maintain quality of life.
Frequently Asked Questions (FAQ)
What is Stage 3 CKD?
Stage 3 CKD is a moderate level of kidney impairment with an eGFR between 30-59 mL/min/1.73 m². It often shows noticeable symptoms and requires careful management to prevent progression.
What are the common symptoms of Stage 3 CKD?
Common symptoms include fatigue, swelling in the legs and ankles, changes in urination, shortness of breath, and lower back pain.
How is Stage 3 CKD diagnosed?
Diagnosis involves blood tests to measure eGFR and creatinine levels, urinalysis to detect protein or blood, and imaging studies like ultrasounds. A kidney biopsy may be used in some cases.
What are the causes of Stage 3 CKD?
Key causes include diabetes, high blood pressure, chronic glomerulonephritis, and polycystic kidney disease.
What risk factors contribute to Stage 3 CKD?
Risk factors include a family history of kidney disease, older age, obesity, smoking, a sedentary lifestyle, and conditions like high blood pressure and high cholesterol.

Pingback: what is chronic kidney disease helpful tips